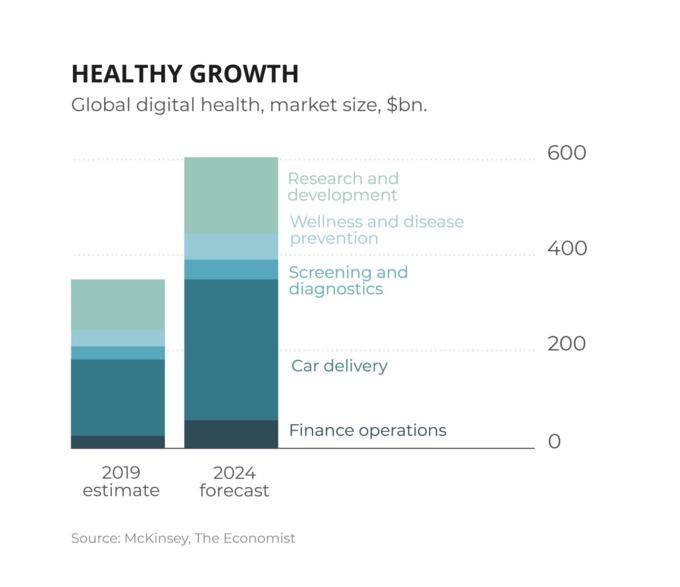
The Healthcare System is Bound to Change Profoundly – From Reactive to Proactive
The COVID-19 pandemic has placed unparalleled demands on the healthcare sector. To address these demands, Healthcare (as well as other) organizations around the world are turning to tech to help meet capacity challenges, accelerate the search for a vaccine, and transition to telehealth.
In this aim, state-of-the-art technologies provided by visionary startups are finally given the attention they deserve, ranging from Automated Data/Imaging Analysis over Telehealth and Digital therapy support to Organoids and Biomarker libraries. Reflecting this momentum, healthcare companies raised more than $18B Q3 2020.
While this trend might be triggered by the current global situation regarding Covid, it also uncovers the historic prioritization of digitalization, as well as the lack of resources and governance provided in fostering system change.
In addition to that, it is coming at a time, when pharmaceutical companies themselves, among others in the Healthcare sector, are facing disruption, dealing with complex supply chains, new models for engagement with healthcare professionals, a largely remote workforce, and new developments in clinical trials. Hospitals are bound to deal with evolving protocols while maintaining continuity of care for others, often against the backdrop of vulnerable staff, supply and equipment shortages, and, for some, accelerating financial headwinds.
This article intends to do three things: Firstly, highlight the significant advancements made across the healthcare sector, accelerated through the pandemic. Secondly, urge health systems to adapt to the current technological healthcare advancements. Thirdly, serve as a reminder that even with a suitable vaccine for COVID-19, there is a lot of room for improvement due to technological advances in the health care sector. We need to continue to innovate in order to be able to deal with future challenges much more efficiently.
Generally, we believe that the pandemics’ unprecedented impact on conventional healthcare systems and the ongoing strive to innovate reinforces our prediction that looking into the future, healthcare will move from a reactive to a preventive approach, and tremendously towards offering personalized treatment enabled through the vastness of new patient data available.
Patient-Doctor Interactions
If the global pandemic has highlighted anything, it is the value of high-quality remote care solutions. As the global workforce experiences the use of new systems and ways of working, it is becoming clear that digital health is also re-defining the doctor-patient relationship.
Digital Health Consultations
COVID-19 has caused a massive acceleration in the use of telehealth, which has helped expand access to care at a time when the pandemic has severely restricted patients’ ability to see their doctors.
Remote patient care is the obvious COVID-19 use case and has seen according growth: Treatments on Munich-based Teleclinic have grown 250% since January, Swedish KRY grew appointments in Germany by 350% from February to March, and the patient/doctor matching platform Jameda claims that demand grew by more than 1000% since March. Apart from general consultation, demand is also growing in niche segments along pregnancy and postpartum health, online dermatologists or mental health.
Yet, changes in Germany - even amidst the crisis - are coming at a slower pace. In order to boost market education, the Swedish remote patient care App Kry, as well as doctor booking platforms like French Doctolib and German Jameda are offering free software solutions for doctors and nurses. While adoption might still be slow, the legislative grounds have been cleared with the Digital Healthcare Act, passed late last year, allowing doctors to prescribe digital health apps to patients, offer online video consultations and write e-prescriptions — and be reimbursed for doing so. While this has been possible for privately insured patients for longer, the Digital Healthcare Act unlocks a 73 million market of publicly insured patients to telehealth providers.
Telehealth has massive potential for revolutionizing the health care system on both patient and payer/provider side. On the patient side it can provide faster access to specialists, emergency and primary care. Patients in rural areas are benefiting from increased accessibility, smaller hospitals from telehealth outsourcing to specialists and better diagnosis. At the same time, team-based, ongoing and value-based care is improving chronic disease management and patient outcomes.
For Payers/Providers, especially post-discharge online care and remote monitoring provide strong cost-cutting potential and at the same time dramatically improve patient well-being.
Current developments are aiming to replicate a doctor’s visit even closer by allowing for digital examinations/ symptom analysis. While Amazon is seeking to have its virtual assistant Alexa record and analyse coughing, MIT researchers have made progress in training an AI model that distinguishes asymptomatic people from healthy individuals through forced-cough recordings through web browsers and devices such as cellphones and laptops.
Israel Medical Center Sheba and Tyto Cares are providing at-home special stethoscopes that both listen to patients’ hearts and transmit images of their lungs to a care team that can intervene as appropriate. US-based Teladoc offers patients smart devices for general care and chronic disease management that are analyzed by their own doctors. Apple also sees a promising future in the healthcare sector, underlined by the increasing health features the Apple Watch offers.
The actions taken by healthcare leaders today will determine if the full potential of telehealth is realized after the crisis has passed. These actions include finding new ways of working for a broad set of providers, improving information exchange, broadening access and integration of technology, implementing new reimbursement schemes and aligning the interests of all stakeholders.
Digital Therapeutic Support
Hundreds of millions of people around the world were suffering from common mental health issues including anxiety, and depression even before COVID-19, but this number has escalated as a result of the pandemic. Yet, demand for mental health services is far outstripping the available supply of trained professionals.
While companies have been working in the space for years, the demand surge due to COVID-19 could accelerate the adoption and once again highlight the tremendous potential that these technologies can have in bridging the demand gap, increasing patient monitoring, and thus, preventing worsening conditions and improving patient well-being. In order to accommodate the COVID-specific disease symptoms, companies have moved ahead to create new health models measuring vital parameters to predict the infection and monitor how the disease and the patient’s health evolves.
Next to digital therapeutic support in mental illnesses, various diseases can now be accompanied by digital health solutions such as Diabetes, Obesity or Hypertension fostering patient’s program adherence, education and monitoring.
Adjacent markets targeting prevention of mental health have also seen tremendous growth - Mindfulness and Meditation startup Headspace with 65 million users in 190 countries landed $140 million to continue building its mindfulness and meditation application.
We believe that digital therapeutic support will create tremendous value in accelerating efficiency, safety and predictability along the diagnostic, treatment and monitoring of patients across different diseases - ultimately, improving patient outcomes and strengthening patient-doctor interaction, while providing cost efficiencies and opening up additional revenue streams to payers.
Nursing & Care
COVID-19 also accelerated the passive monitoring of patients through wearables as well as contactless, passive biometrics to reduce healthcare workers’ risk of exposure to the virus. These developments open up the potential for significant facilitation in one of the problem sectors of most modern healthcare systems: Nursing & Elderly care.
While the wearables’ development allows for an active monitoring via essential parameters, the passive monitoring does not necessitate patients to wear e.g. a tracker but instead uses sensors and machine learning to detect patients positioning in the room.
Emerald, a device recently developed by MIT researchers, is installed in hospital rooms and collects signals which are then analyzed using machine learning. In doing so, the device is capable of differentiating between patients in a room by their movement patterns, sensing people through walls, and is sensitive enough to capture subtle movements such as the rise and fall of a patient’s chest to analyze breathing patterns. While Emerald is installed covering the room, Israel-based EarlySense develops sensors that can be attached beneath hospital mattresses or chairs. Data and alerts are sent to hallway monitors or handheld devices.
Passive monitoring tools can reduce the pressure on nurses and caregivers as well as increase early detection of disturbances. But innovation in elderly/patient care doesn’t stop there. There is also room for improvement in embracing relevant gaps in patient & family disease education, providing Health status dashboards for patient families or developing Virtual Reality Companions, just to name a few.
While these measures might sound minor at first, giving the elderly the ability to life more independent lives can have tremendous benefits for their overall health, while reducing workload and risk for care personnel.
Nevertheless, its success does not only depend on payers and clinicians, but also on caretakers who are using collaboration tools to reduce workflows, protect high-risk patients and collect data for clinicians.
Computer Assisted Data Collection & Diagnosis
Using computer-vision to accelerate diagnostics has been around for years, but it has found a new and prominent application in the pandemic. Startups such as Mumbai-based Qure.ai, that raised 16 Million from Sequoia Capital India, is using its deep learning technology to undergo X-ray screening for COVID-19 symptom detection and prediction of a COVID-19 risk score.
Next to significant support in the diagnosis, US startups have also started using government data as an input to their models in order to supply predictions for containment areas and the spread of the infection. While this is a successful example of data provision and collaboration, hospitals and academia often are reluctant to share their data with other parties in order to publish results first. How critical collaboration on patient data is, is strongly exemplified by this crisis - demanding a collaborative attitude to fight a pandemic that does not stop at borders.
This is even more important given the vastness of additional clinic data being generated through for example wearable devices, necessitating a collaborative strategy to bridge the ‘valley of death’ of translational medicine and provide the grounds for precision medicine.
While the application of e.g. AI in accelerating diagnostics, testing or characterization of diseases is endless, we selected a few key areas to look into more detail.
Medical / Scientific Image Analysis
Computer vision to detect anomalies in medical scans and aid in disease diagnosis is probably the most straight-forward application of AI saving both time and costs as well as increasing early-stage disease detection. Its application allows the shift of an error-prone process that is dependent on Radiologists expertise and full concentration, towards a (partially) automated analysis supporting the Radiologists in providing the final diagnosis.
Within this field of early detection and characterization of diseases, companies are experimenting across four dimensions. As mentioned above, the most used application of Data Vision in medical imaging lies in the disease diagnosis.
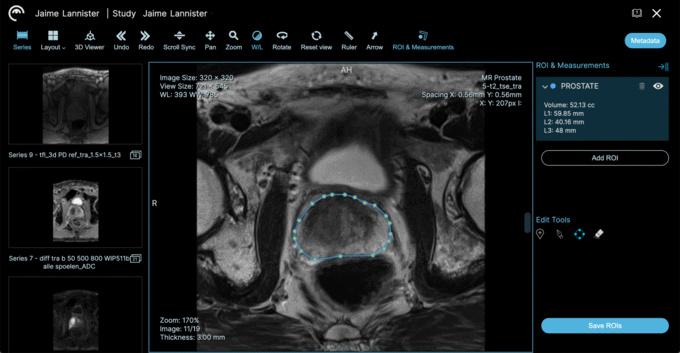
Prostate analysis powered by Ezra's AI engine. Source: ezra.com
The next wave of radiology AI applications is moving beyond disease diagnosis to image enhancement — the process by which the radiology scans are obtained in the first place. The goal: Using AI algorithms to generate high-resolution CT or MRI scans with much fewer data than required to expose patients to lower levels of radiation. Facebook’s joint research with NYU Langone Health uses AI to construct high-quality MRI images using a quarter of the data, thereby significantly reducing MRI scanning times and associated costs while increasing capacity.
Going yet in another direction is startup Subtle, which is working on AI-based image enhancement for faster and higher-quality PET and MRI scans.
Lastly, AI usage in Image Analysis can facilitate less invasive diagnostic procedures. New-York-based startup EZRA aims at detecting cancer early by regular MRT scans that are enhanced by their data treasure. Patients can undergo regular scans at EZRA to detect early signs of cancer in 13 different organs. Their prostate scan recently received FDA-clearance.
These developments exemplify the tremendous potential of computer-assisted diagnosis in creating substantial patient benefits such as reducing patient waiting times for imaging and exposure to radiation and substantially increasing early stage/right disease detection. Additionally, it allows a higher patient throughput on diagnostic devices, reduced interpretation efforts and associated time/cost savings. Yet, medical image analysis is not bound to radiology, but is applied along different use cases, e.g. in analyzing lab data at Universities/R&D sites.
Wearables & Digital Biomarker Analysis
Wearables were already on the up before the pandemic began, but research by GlobalData estimates that the market is now on track to increase from being worth nearly $27bn in 2019 to $64bn by 2024. The surge is partially triggered by a greater awareness of people to health monitoring due to COVID-19 but also by technological advancements of smart wearables. The devices used can differ from smart rings, trackers and smart textiles to any combination of electronic component and app.
Next to wearables, health apps are leveraging smartphone microphones and sensors to gather data. One example is Mindstrong, an app provider that pairs patients with a network of providers to deliver personalized mental health care, utilizing a digital biomarker tracker of mood and cognition via patterns of smartphone interactions. Other providers are tracking vocal biomarkers of depression or dementia through the automated analysis of voice features and cognition, such as voice tremor, vocabulary, semantic qualities. As thresholds are overcome/ defined signs of depression detected, the results are marked to be alarming in psychiatrists/support dashboards allowing for immediate interaction.
This automated analysis can be used in multiple stages e.g. in diagnosing mental illnesses, bridging the timely gap between detection and counseling, as a support tool during therapy itself or in monitoring the patient after finishing a therapy.
The potential of data collection through wearables and apps and the subsequent analysis of digital biomarkers is immense, significantly shifting healthcare from a reactive to a more preventive approach, as more and more data will be available to analyze and predict future health outcomes.
Precision Medicine
The goal of precision medicine is to provide the right treatment at the right time for every patient – with improved diagnostic accuracy, more personalized treatments, the elimination of unwarranted variations, and advanced therapeutic outcomes. The COVID-19 crisis has illustrated with clarity the importance of each of these efforts. Since the beginning of the pandemic, startups, universities, and big pharma have used AI to better understand the structure of the novel coronavirus, identify promising new compounds for treatment, find existing FDA-approved compounds that can be repurposed, and even design drug molecules that are structurally stable.
Recursion Pharma has also released massive SARS-CoV-2- related datasets publicly. Recursion has decided to use AI to better understand the virus. In a controlled environment, healthy cells were infected with the SARSCoV-2 virus, and the microscopic images were analyzed using deep learning to identify the physical changes that occur in these cells as a result of the infection. The San Antonio Partnership for Precision Therapeutics has announced the funding of three projects that will accelerate treatments for COVID-19 using precision medicine principles to better understand COVID-19 susceptibility, measure its impact, and discover potential therapies.
This exemplifies the discussed importance of the availability of data not only for improved diagnosis, but also to prepare the grounds for personalized treatment. While e.g. wearables and health tracker are contributing to the vastness of medical data, the aggregation and integration of all relevant data points is still lagging behind, thereby, hindering researchers/clinicians to close the loop to fully understand patients from their symptoms, to treatment, to outcomes.
Yet, in some instances, everything’s coming together. Swiss pharma giant Roche now has it all: Through the acquisition of Cancer-research company Flatiron Health and their remaining stake in Molecular-insights company Foundation Medicine, it now has access to genomic data from thousands of oncology patients. Combining this data with innovative, targeted therapies could provide Roche with a continuous data loop from identifying a patient, confirming genomic signature, treatment selection, and on to monitoring outcomes.
Nevertheless, research claims that genomics has underdelivered for precision medicine and that moving closer towards precision medicine will require integrating genomics with other “omics’’ – transcriptomics (RNA), proteomics (proteins), and metabolomics (metabolites) to improve how we analyze and utilize biological information. We believe that relevant developments along these lines will be proteomic biomarker analysis, the implications of protein folding insights and the development of easy-to-use organoid models.
Protein Folding
Proteins are supporting practically all body functions. They are large complex molecules, made up of chains of amino acids. What a protein does, and how it does it, depends also on how it folds up after its creation, into its final, intricate shape. Figuring out exactly the shape that proteins fold into is known as the “protein folding problem”. In a paper published in Nature, researchers at DeepMind, an artificial-intelligence laboratory owned by Alphabet, show that they made enormous progress on one of biology’s grandest challenges—how to use a computer to predict a protein’s shape from just a list of its amino-acid components.
If this is scalable, it would mean that the currently employed, timely processes of probing protein shapes through techniques like x-ray crystallography can be replaced with a few hours of computing time while ensuring approximately the same accuracy. This development would truly be one-of-its-kind, solving a decade-encompassing grand challenge and providing tremendous value throughout various biological disciplines/research streams.
The significance of this change can be seen in an acceleration of drug development and a potential cure for diseases with their origin in single misshapen proteins. Depending on how DeepMind decides to license the technology, research sees additional potential in the vastness of not yet structurally-determined amino acids. The analysis of those could facilitate the screening of drug candidates to see which are likely to bind well to a particular protein, re-analyse existing drugs for additional functions, and boost synthetic biology, by speeding up the creation of human-designed proteins intended to catalyse chemical reactions.
Some promising successes have already happened. During the pandemic, DeepMind successfully used AlphaFold to predict protein structures associated with COVID-19 and publicly released this data.
Organoids
We believe that the road to precision medicine is also facilitated by another development: The newly learned ability to culture organ-specific tissue from cells. Organoids are tiny, self-organized three-dimensional tissue cultures that are derived from adult stem cells of organs or tumors. Such cultures can be crafted to replicate the complexity of the cells they are derived from, such as mimicking the functioning of lung, gut or cancer tissue.
Organoid technology opens a range of untapped opportunities for the study of organ or cancer interaction with specific drugs or antibodies. Organoids will thereby provide the grounds for specific disease models and accelerate drug development and testing as well as creating more accurately-targeted drugs. To date, cell tests within the drug development process have relied upon animal models and human cell lines that have little resemblance to normal or diseased tissue - one potential reason behind the high failure rate of clinical trials, adding to the high cost of drug discovery.
The most exciting part about organoids are the use cases in precision medicine. For example, if a patient suffers from breast cancer, there are many possible drugs that could be used to cure that disease. However, today it is largely unclear why a specific drug works at one patient but not at the other. With breast cancer organoids directly grown from patient cells, the potential drugs can be tested on a patient’s real cells in the laboratory. Only the drug that works best at a patient’s organoids will then be used on the patient herself. Last but not least, organoids lay the foundation for treating patients with their own immune cells. It can be tested in a lab environment which immune cells of a patient work best on the specific disease. These immune cells can then be propagated and re-injected into the patient.
In the long run, cultured mini-organs may replace transplant organs from donors. However, currently specific growth factors, that are derived from mice which have a special kind of tumor, are needed to grow organoids. As long as no solution for this is found, organoids will hardly be implanted into humans. We believe that organoids will be a key enabler for developments in the area of drug targeting and precision medicine.

Organoids grown with Sun Bioscience patented technology.
Source: Sun Bioscience / Venturelab
Proteomic Biomarker Analysis
Advances in genome sequencing have greatly propelled the understanding of the living world - however, it falls short on allowing a full description of a biological system.
Focusing on proteomics has emerged as another large-scale research stream for improving the understanding of biology. Proteomics is concerned with studying the whole protein repertoire of a defined entity - a biological fluid, an organelle, a cell, a tissue, an organ, a system, or the whole organism. Advances in proteomics methods offer many promising new directions of studying in clinical fields such as the proteomic biomarker discovery and drug targeting.
The proteomic biomarker discovery is advanced in various diseases such as cancer, cardiovascular diseases, AIDS, and renal diseases which provide non-invasive methods by the use of body fluids such as urine and serum. Hence, in the instance of cancer, in-depth studying of proteomics profiles of various specimens obtained from cancer patients are expected to increase our understanding of tumor pathogenesis, monitoring, and the identification of novel targets for cancer therapy.
Tapping into the market of precise, patient-centric drug development, British startup Ilof is developing a platform for diseases biomarkers and biological profiles. If successfully employed, techniques as such can significantly increase trial outcomes by using the right candidates for clinical tests, and improve and accelerate diagnostics. While Ilof currently focuses all its efforts on developing this platform in an aim to accelerate the drug development for Alzheimer’s, their library is intended to bring the power of technology to other diseases such as Digestive Cancer, Stroke and Infectious diseases.
In fact, one of the main objectives of proteomics is to identify and discover the disease-related biomarkers and drug targets. Because of many confronting factors, such as the complexity of body fluids, and low abundance of a protein biomarker, there are many challenging steps for biomarker discovery to validate. Despite the existing challenges, there are other “omics” methodologies such as peptidomics, and metabolomics along with bioinformatics methods to help the systematic study of a disease for ideal biomarker introduction.
Summary & Outlook
In summary, we believe that an extension of genomics towards “omics” will lead to an even better understanding and actionability of insights derived, paving the way towards delivering the ultimate in high-value, patient-centered care by enabling the right treatment to be given to the right patient at the right time.
Overall, we believe that the innovation sweet spot for Freigeist Investment cases will center around the interface of Software and Hardware/Medical Research.
Investment cases will concern companies, which put technology at the core of their solution thereby solving a critical inefficiency in the healthcare provision. An example for such a company is Alphafold, that is applying its AI Algorithms to solve a decade-preserving challenge of determining the structures proteins fold into. In terms of the specific functional area of investment, Freigeist believes in the immense transformation of the healthcare sector through personalized medicine. Hence, there will be a strong emphasis on investing in enabler technologies supporting this development.
Moreover, we are convinced that our healthcare sector will transform from reactive to proactive. Regular screenings of e.g. our fluids for disease biomarkers in connection with more health data from wearables will allow us to dramatically improve and prepone diagnoses, thereby saving millions of lives.
We, at Freigeist believe that the healthcare sector is bound to be changed and technological advancements will be the key driver of that change. While COVID-19 is definitely not the origin of innovation in healthcare, it has shown the magnitude of change possible - if bureaucracy is reduced, innovation capabilities are fostered and fundamental change is cherished.
This article was written with the help of Louisa Bracht